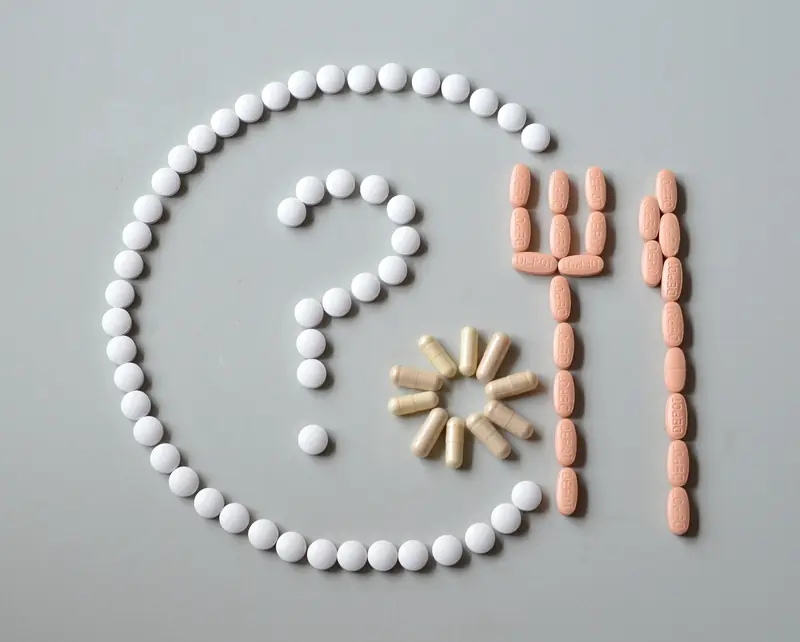
When taking pills with food, we often overlook their interactions. However, these interactions involve chemical reactions.
Proteins, Fats, Carbohydrates vs. Steroids, Analgesics, Antibiotics
The combination of food and medication can be either beneficial or explosive.
Proteins
Doctors advise against combining pills with protein-rich foods such as meat, nuts, cheese, and beans. Proteins react instantly with medicinal components, potentially reducing the effectiveness of the medication.
Fats
If you take medication and then eat a steak, the drug will take longer to take effect. This delay can be critical when you’re dealing with a headache. Waiting half an hour after taking medication before eating can help alleviate the pain more quickly. An exception is fat-soluble vitamins (A, E), which are better absorbed after a hearty meal.
Carbohydrates
The ideal companions for pills are found among fruits, vegetables, grains, pastries, and pasta. Carbohydrates harmonize well with medications, ensuring optimal absorption.
Antibiotics
Antibiotics work well when taken with rosehip tea, as vitamin C helps the body recover from illness more quickly. Your body will also need vitamin B12, folic acid, and ascorbic acid, which you can get from walnuts, fish, brown rice, white beans, and broccoli. After completing a course of antibiotics, it’s essential to take probiotics for two to three weeks. You can supplement these with bio-yogurt, soft cheese with mold, bran, and sauerkraut.
Analgesics
Taking painkillers can lead to a loss of vitamin C, iron, folic acid, and zinc in the body. You can replenish these micronutrients with pumpkin seeds and cabbage. Young lamb, grapefruits, and oranges can also help.
Steroids
If you’re treating eczema, rheumatoid arthritis, or bronchial asthma with steroid medications (like prednisone or hydrocortisone), you may experience a decrease in vitamins C, B6, D, K, as well as zinc and magnesium. Including sweet peppers, lentils, soy, barley, and oatmeal in your diet can help remedy this situation.

List of Medications That Should Not Be Mixed with Alcohol
Alcohol is toxic to the body, and poisoning never has a favorable outcome.
The severity of the consequences:
- Combining alcohol with medications can lead to dizziness, headaches, blood pressure spikes, behavioral changes, nausea, vomiting, and fainting;
- It may intensify side effects;
- Alcohol interaction with nitrates can sharply lower blood pressure;
- Consuming alcohol while taking acetaminophen and other painkillers can cause liver damage;
- Taking non-steroidal anti-inflammatory drugs (NSAIDs) alongside alcohol increases the risk of gastrointestinal bleeding;
- Contact between ethanol and active drug ingredients can weaken or enhance their effects;
- Combining alcohol with sedatives, antidepressants, and antipsychotics raises the risk of coma and cardiac arrest.
It is strictly forbidden to mix alcohol with:
- Barbiturates, sleeping pills, and tranquilizers (consequences range from lethargy and fainting to respiratory depression and death);
- Antibiotics (alcohol significantly reduces the effectiveness of antibacterial agents and turns them into toxins);
- Non-steroidal anti-inflammatory drugs (risk of gastropathy and ulcer development with a chance of gastrointestinal bleeding);
- Acetaminophen (dangerous for the liver – hepatotoxicity);
- Blood pressure medications (antihypertensives combined with alcohol can cause dizziness, arrhythmia, and fainting);
- Cholesterol-lowering medications (mixing alcohol with hypolipidemic agents dangerously increases the load on the liver);
- Antihistamines (allergy medications increase the load on the central nervous system and exacerbate alcohol intoxication);
- Antifungal agents (antiprotozoal tablets block the enzyme alcohol dehydrogenase in the body, preventing ethanol breakdown, which poses a risk of alcohol poisoning with fatal outcomes).
As you can see, drinking while undergoing treatment is a bad idea. To put it bluntly, it’s downright crazy.

Which Medications Should Not Be Taken Together?
It is crucial to inform your doctor about any additional prescriptions to avoid incompatible combinations of medications.
Verapamil – with Beta-Blockers
Simultaneous use of antihypertensive medication and heart failure drugs (like atenolol, metoprolol, etc.) can be deadly. A calcium blocker for treating ischemia, when combined with beta-blockers, can slow the heart rate to the point of cardiac arrest.
Solution: When prescribed both medications, monitor your pulse, and if it drops to 50 beats per minute or less, consult your doctor.
Aspirin – with Ibuprofen
Aspirin, which thins the blood, should be approached with caution: it not only prevents blood clots but also irritates the stomach lining. Non-steroidal anti-inflammatory drugs (NSAIDs) have the same characteristic, so regularly taking ibuprofen with aspirin will inevitably provoke gastrointestinal bleeding (the same effect occurs with the combination of antidepressants and NSAIDs). In pharmacokinetics, NSAIDs compete with aspirin for the same enzyme but block it less effectively than aspirin. Ultimately, this combination reduces the effectiveness of the heart medication.
Solution: Do not take aspirin and ibuprofen simultaneously or on an empty stomach. It is safer to take NSAIDs half an hour after aspirin or eight hours before. It’s simpler to replace ibuprofen with acetaminophen.
Anticoagulants – with Painkillers
NSAIDs have a side effect: they reduce blood clotting. Anticoagulants, which also reduce clotting, share this quality. Therefore, warfarin should not be taken with ibuprofen if you want to avoid uncontrolled bleeding.
Solution: When taking anticoagulants, acetaminophen can be an acceptable painkiller.
Antihypertensives – with NSAIDs
This combination can lead to two undesirable outcomes. Due to increased arterial tone and fluid retention, NSAIDs reduce the effectiveness of antihypertensive medications and exacerbate hypertension. In addition to hindering the hypotensive effect of diuretics, the simultaneous use of NSAIDs and antihypertensive drugs increases the risk of acute kidney failure.
Solution: Replace NSAIDs with acetaminophen.
Antibiotics – with Oral Contraceptives
Intestinal microflora is involved not only in digestion but also in the biotransformation of hormones. By disrupting the natural microbiotic environment, antibiotics also affect biotransformation. Taking antibiotics with birth control pills reduces the effectiveness of contraceptives, potentially leading to unwanted pregnancies. Furthermore, antibiotics block liver enzymes, resulting in decreased blood concentrations of contraceptives and reducing their ability to prevent pregnancy.
Solution: During antibiotic treatment, use condoms and other alternative contraceptive methods.
Loperamide – with Calcium
Both medications slow down intestinal peristalsis, and when combined, they double the likelihood of constipation.
Solution: If you are taking loperamide for diarrhea, refrain from treating osteoporosis with calcium medications during this time.
Cold Medications – with Allergy Medications
In powdered soluble “teas,” alongside analgesics and vasoconstrictors (like acetaminophen and phenylephrine), there is also an antihistamine component that reduces tearing and sneezing. Adding a separate allergy medication will decrease concentration and lead to drowsiness, which is dangerous when operating machinery.
Solution: During treatment for acute respiratory viral infections (ARVI), stop taking antihistamines or choose modern medications from the latest generations with less impact on the nervous system.
Statins – with Antifungal Agents and Macrolide Antibiotics
When erythromycin or clarithromycin encounters statins, or when statins meet antifungal medications like fluconazole, Diflucan, or Flucostat, the action of liver enzymes that process statins is inhibited. This leads to an excess of substances in the body that can harm muscles.
Solution: It’s best to avoid taking statins altogether. However, if you are already taking them, do not abruptly stop to avoid withdrawal syndrome. Completely discontinuing statins during treatment with antifungal medications or antibiotics will cause a spike in cholesterol levels. You should taper off statins gradually, reducing the dose by one-third or half while simultaneously taking omega-3 (starting with 2 grams of fatty acids and later increasing the dosage to 3 grams).
Levothyroxine – with Statins, Raloxifene, Iron, Calcium, Magnesium, Estrogens, and Proton Pump Inhibitors
The listed medications hinder the absorption of thyroid hormones, which can provoke hypothyroidism in patients undergoing replacement therapy. Additionally, estrogens, through connective action, necessitate an increase in hormone doses.
Solution: Inform your doctors about taking levothyroxine (Euthyrox) for dose adjustments.
Tetracyclines – with Antacids, Iron, and Calcium
It is important to consider that antacids reduce the absorption of antibiotics. The tetracycline class of antibiotics, when combined with iron supplements, weakens each other’s effects, while insoluble calcium salts accumulate in the body when taken together.
Solution: The course of antibiotics does not allow for undesirable “neighbors.” You should avoid incompatible companions during antibacterial therapy.

What Should Not Be Taken with Iron
When taking multivitamins, check for the Fe component. If iron supplements are included in your prescriptions, you need to know when to take them in combination therapy: before or after other medications (and how many hours or minutes should separate the doses). The reason is that iron reacts with many medications, affecting their effectiveness, and vice versa. For instance, medications containing medical cholesterol (like cholestyramine and colestipol) hinder iron absorption. Acid blockers (like cimetidine, famotidine, and ranitidine) have a similar effect. Iron also interferes with the absorption of antibiotics (quinolones and tetracyclines) and complicates the action of inhibitors of the corresponding enzyme when taken with blood pressure medications. Iron supplements can lower thyroid hormone levels and reduce the effectiveness of Parkinson’s disease medications (like carbidopa and levodopa). Additionally, contraceptive pills can increase iron levels in the body.
Antibiotics: Before or After Meals
The most crucial aspect of antibiotic treatment is strict adherence to the rules of administration. Violating the timing, duration, and dosage weakens the drug’s effect, intensifies side effects, and fosters bacterial resistance to medications. However, it is equally important to follow the timing of taking the antibacterial agent: before or after meals. This is specified in the medication instructions for a reason: food intake affects the absorption of the chemical substance in the gastrointestinal tract. Some antibiotics are better absorbed before meals, while others are more effective after.
Medications that irritate the stomach lining should be taken after meals and washed down with plenty of still water.
The stated frequency of administration indicates an 8-hour interval for three doses and a 12-hour interval for two doses. To restore the natural intestinal microflora, probiotics (fermented dairy products) should be taken separately from antimicrobial medications. Antibiotics require adherence to a special diet: fatty, fried, smoked, canned foods, as well as acidic fruits and alcohol should be excluded from the diet. Food should not overload the liver, as antibiotics suppress its function. During treatment, sweet fruits, vegetables, and white bread can be included in the diet.
Vitamin D and Dairy Products
People with congenital lactose intolerance (the sugar found in milk) are prone to vitamin D deficiency in their bodies. The reason for the impaired absorption of the carbohydrate found in milk, butter, and cheese lies in the insufficient amount of the enzyme lactase in the small intestine, which breaks down lactose. Within two hours after consuming dairy products, individuals with intolerance experience abdominal pain, bloating, diarrhea, gas, and nausea. Clearly, those with digestive disorders should avoid dairy products.
However, dairy is a valuable dietary source of vitamin D. It contains several micronutrients of various origins. While cholecalciferol (D3) is produced in our bodies under the influence of ultraviolet light, ergocalciferol (D2) is found only in food and enters the body through diet. In conditions of limited sunlight and a restricted diet, we find ourselves defenseless against osteoporosis and rickets. The “sunshine vitamin” keeps teeth and nails healthy, as it regulates phosphorus and calcium metabolism, thus supporting bone health. Additionally, vitamin D boosts the body’s defenses, strengthens the nervous system, and helps prevent the development of cancer and autoimmune diseases.
So how can we regulate our intake and compensate for the deficiency of this vital component? Special dietary supplements are available. You can buy fish oil and vitamin D supplements in oil and water-based forms at the pharmacy. If dairy products are contraindicated for you, look for vitamin D in plant-based foods (potatoes, parsley, nettle, alfalfa, dandelion, fortified cereals, soy, almond, coconut, or rice milk), meat, fatty fish, eggs, and wild mushrooms.
