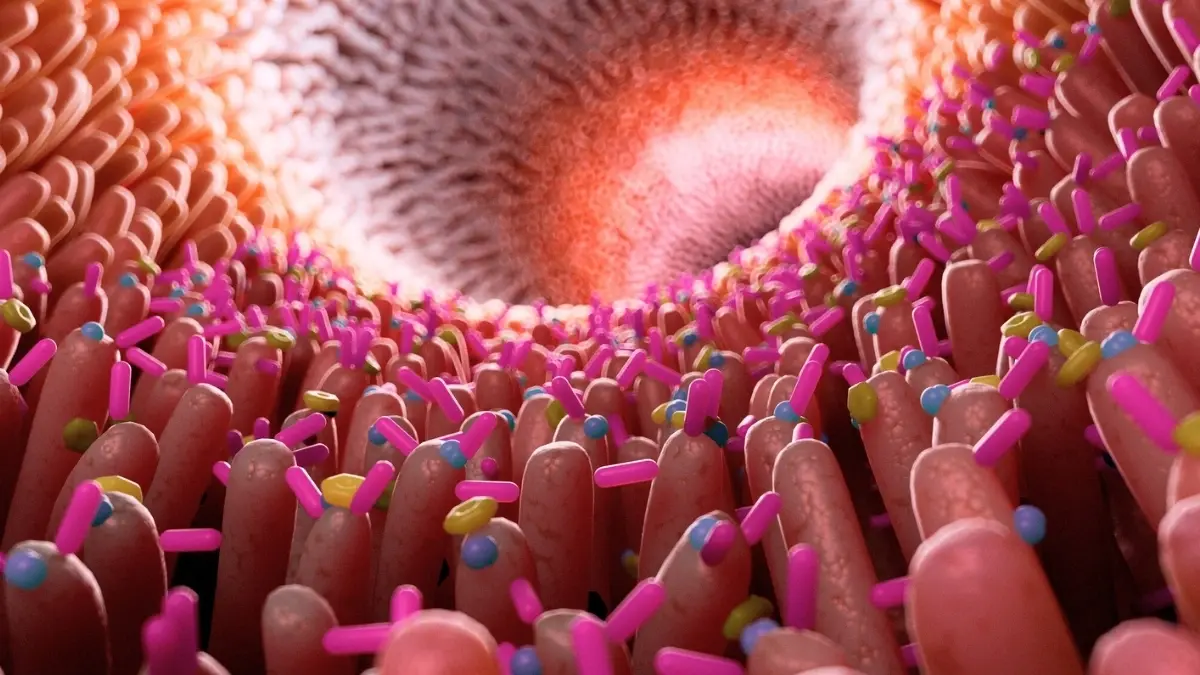
 Previous studies on mice have already shown that may be transmitted to younger individuals through gut microbiota. This has established a connection between the digestive system and brain health.
Previous studies on mice have already shown that may be transmitted to younger individuals through gut microbiota. This has established a connection between the digestive system and brain health.
Now, researchers have confirmed this theory in humans, demonstrating that intestinal inflammation could be a factor that activates this connection. “We found that individuals with Alzheimer’s disease exhibit more pronounced intestinal inflammation. When we analyzed their neuroimaging data, those with greater intestinal inflammation showed an accumulation of amyloid plaques in the ,” noted Professor Barbara Bendlin from the University of Wisconsin.
The team conducted an analysis of fecal calprotectin (a marker of inflammation) collected from 125 individuals participating in cohort studies aimed at preventing Alzheimer’s disease.
Participants underwent several cognitive tests, interviews regarding family history, and testing for the presence of a gene associated with a high likelihood of Alzheimer’s disease. Some participants also underwent clinical tests for the presence of amyloid protein accumulations, a common sign of the pathology associated with neurodegenerative diseases.

While calprotectin levels were generally higher in older patients, this marker was most pronounced in those with characteristic amyloid plaques associated with Alzheimer’s disease.
Levels of other Alzheimer’s disease biomarkers also increased with the progression of inflammation, reported Science Alert.
Interestingly, even participants without a diagnosis of Alzheimer’s disease exhibited poorer memory performance with higher levels of calprotectin.
Preliminary laboratory analyses indicated that chemicals released by gut bacteria may stimulate inflammatory signals in the brain.
The authors of the new study suggested that changes in the microbiome trigger processes in the that lead to systemic inflammation. This inflammation is moderate but chronic, causing gradual, subtle damage that ultimately disrupts the sensitivity of our body’s barriers.
“Increased intestinal permeability can lead to elevated levels of inflammatory molecules and toxins in the bloodstream, which originate from the gut lumen; this will cause systemic inflammation, which in turn can disrupt the blood-brain barrier and contribute to neuroinflammation, potentially leading to nerve tissue damage and neurodegeneration,” stated co-author Federico Rey.
Researchers are now conducting experiments on to determine whether dietary changes that promote inflammation can trigger the development of Alzheimer’s in rodents.
Such research is critically important, especially considering that effective treatment methods for millions of people worldwide suffering from Alzheimer’s disease are still lacking.
The study’s findings were published in the journal Scientific Reports.
Photo: Unsplash
