 Lack of sleep is one of the primary factors contributing to the development of , heart disease, stroke, obesity, and type 2 diabetes. Insomnia also weakens the immune system, making individuals more susceptible to infections.
Lack of sleep is one of the primary factors contributing to the development of , heart disease, stroke, obesity, and type 2 diabetes. Insomnia also weakens the immune system, making individuals more susceptible to infections.
Key symptoms of insomnia include difficulty falling asleep, trouble staying asleep, waking up too early, and being unable to fall back asleep.
Meanwhile, sleep is a vital biological necessity for the body’s recovery. When the cycle of chronic insomnia disrupts this essential restoration, it triggers a cascade of hormonal imbalances, inflammatory processes, and the accumulation of cellular damage.
This domino effect places a burden on the cardiovascular system, disrupts metabolism, and weakens the body’s primary defense mechanisms, turning chronic into a critical risk factor for some of the most severe diseases.
Sleep is also crucial for overall brain health. Nightly rest initiates the process of clearing the brain of waste and toxins that accumulate during wakefulness.
The brain cannot complete this essential process while awake, allowing toxins to build up, including inflammatory markers and proteins associated with Alzheimer’s disease and other forms of dementia. This leads to atrophy in parts of the brain responsible for memory, executive functions, and movement.
What Did the New Study Reveal?
A long-term aging study involving patients at the Mayo Clinic aged 50 and older linked chronic insomnia to accelerated cognitive decline and an increased risk of developing dementia.
By analyzing participant data, researchers found that individuals with chronic insomnia had a 40 percent higher likelihood of developing cognitive impairments. Their brains also showed signs of accelerated aging, as reported by Daily Mail.
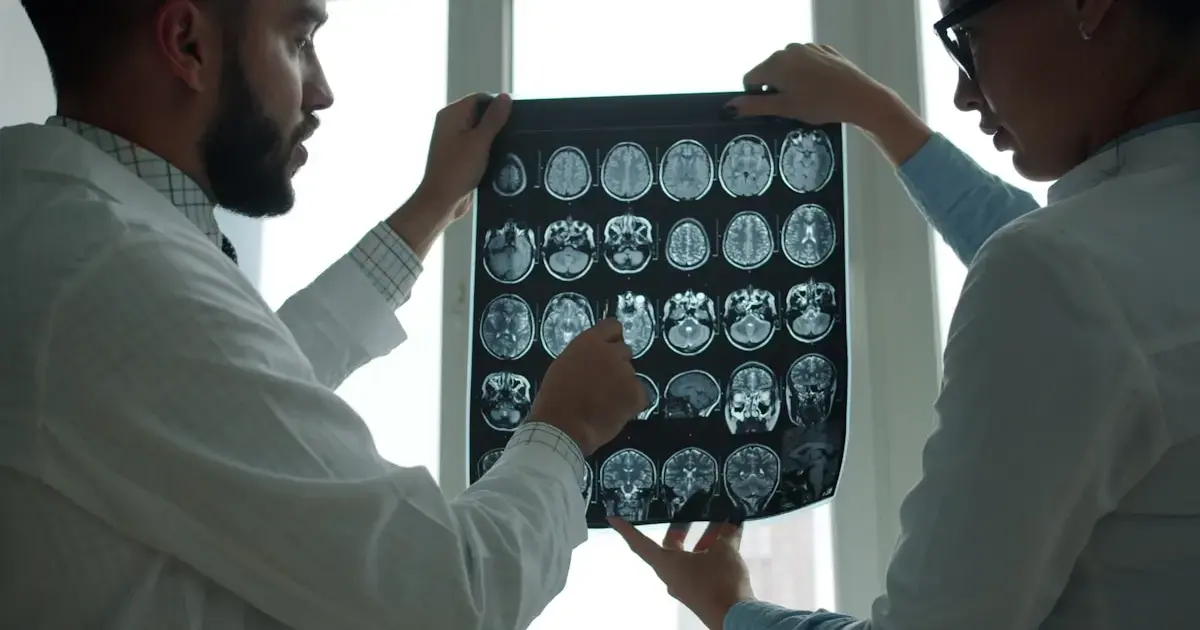
The study connected insomnia with tangible biological damage, including increased accumulation of proteins associated with .
As is known, lack of sleep complicates the removal of beta-amyloid, leading to plaque formation, and may also increase levels of tau protein, which forms toxic tangles.
In carriers of the APOE4 gene, a known genetic risk factor for Alzheimer’s disease, chronic insomnia resulted in an even sharper decline in cognitive functions. About 20-25 percent of Americans have one copy of this gene, while 2 percent have two copies.
These findings suggest that chronic insomnia may serve as both an early warning sign and a potential contributor to future cognitive impairments. The study results were published in the journal Neurology.
How is sleep deprivation linked to deadly diseases?
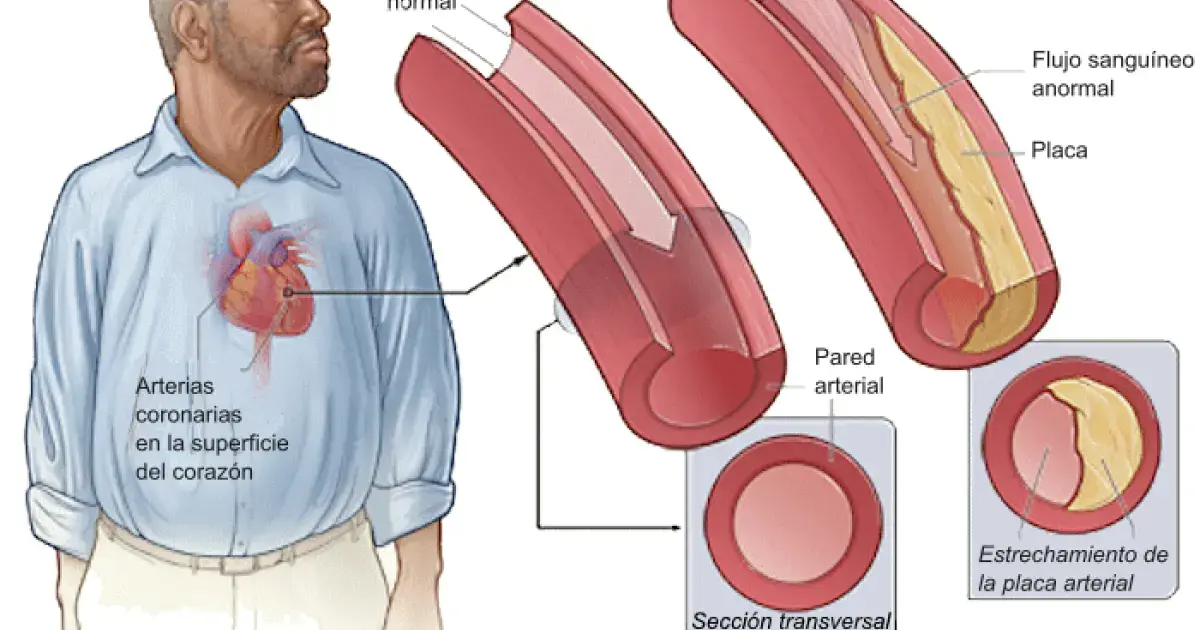
Heart Disease
When the body is consistently deprived of adequate sleep, it enters a state of heightened stress and produces excessive amounts of cortisol. This surplus of the hormone keeps the body in a constant “fight or flight” mode, increasing heart rate and placing undue strain on the heart.
Sleep is also critically important for regulating the immune system. Without it, the body produces an excess of inflammatory cytokines—proteins involved in the immune response. This leads to a state of chronic inflammation throughout the cardiovascular system.
High cortisol levels and chronic inflammation damage the smooth protective lining of blood vessels. This is a primary cause of —a process in which plaques of fat, cholesterol, and other substances accumulate in the arteries. Hardened, narrowed arteries significantly increase the risk of heart attack, stroke, and other cardiovascular diseases.
Hypertension
The primary function of sleep is to give the cardiovascular system a break. In a well-regulated body, blood pressure corresponds to the sleep-wake cycle, significantly dropping at night. This decrease helps the heart work less intensely, allowing the walls of blood vessels and arteries to relax.
When sleep is disrupted, this vital drop does not occur. As a result, the heart and blood vessels are forced to operate at daytime pressure levels 24 hours a day, subjecting themselves to constant strain.
Weight Gain and Obesity
Insomnia and sleep deprivation disrupt the normal production of key that regulate appetite, including ghrelin, which stimulates hunger, and leptin, which signals satiety. The hormonal imbalance that arises from this leads to increased feelings of hunger and decreased feelings of fullness.
Additionally, lack of sleep affects neurological reward pathways. This heightens the sense of pleasure and value associated with high-calorie, carbohydrate-rich, and fatty foods.

Type 2 Diabetes
Insufficient or poor-quality sleep reduces the body’s ability to regulate blood sugar levels, contributing to the development of insulin resistance—the primary risk factor for .
Sleep deprivation lowers the body’s sensitivity to insulin—the hormone necessary for transporting glucose from the blood to cells for energy. To compensate for this reduced sensitivity, the pancreas must produce more insulin to maintain normal sugar levels. This increased demand over time leads to pancreatic overload.
can exacerbate inflammation throughout the body. Weight gain and inflammation are well-known factors that enhance insulin resistance. This creates a dangerous cycle that significantly increases the risk of developing type 2 diabetes and other metabolic disorders.
Photo: Openverse, Unsplash
